- May 14, 2019
How to Describe Your Pain to a Doctor
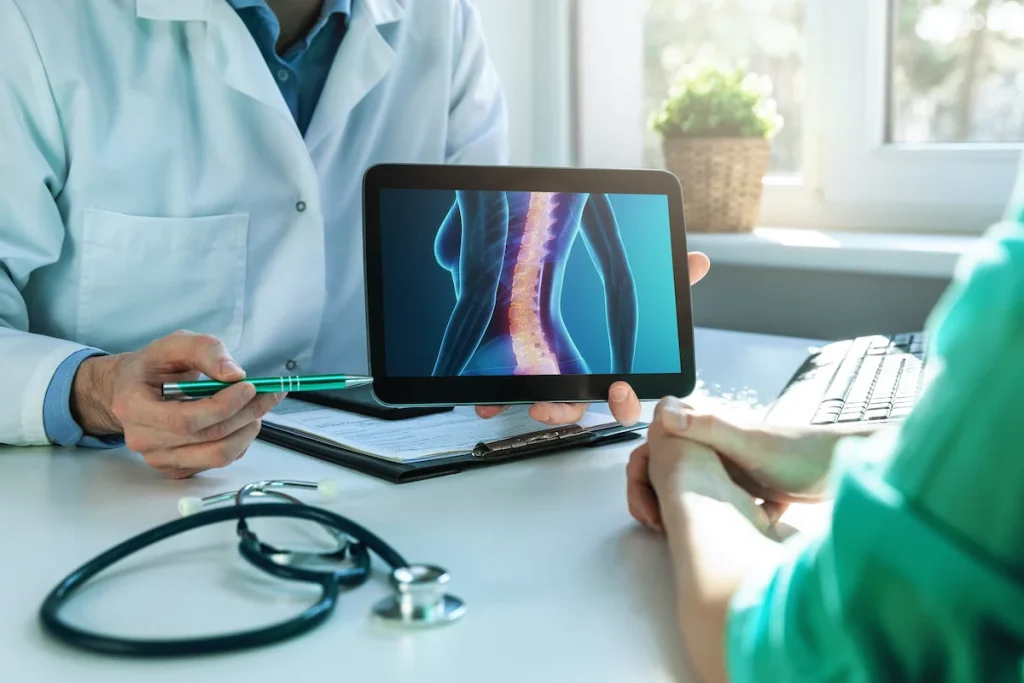
As many chronic pain patients know, it can be difficult to describe pain to someone who is not experiencing it. When this results in misunderstanding between family members and friends, it can be frustrating. When this results in miscommunication with doctors, it can be devastating. It’s easy to feel hopeless when it seems like the one person who may be able to help you doesn’t understand your pain. In some part, this disconnect is due to general practitioners lacking experience with chronic pain. It is also a result of the complex nature of pain.
With a broken leg, a simple physical examination can reveal the extent of the injury and sometimes even its cause. With pain, things are a lot more complicated. Each person’s experience of pain and tolerance of that pain is different, so what someone might describe as a six on the pain scale, someone else might describe as a two.
To develop an effective treatment plan, patients and doctors need to work together to establish clear communication and bridge this gap. Aside from the traditional 1-10 pain scale, there is also the LOCATES scale. This scale was developed by the American Pain Foundation. Rather than simply assessing the severity of the pain, it digs deeper into the details.
It reminds people to report on the location of pain and whether it moves around the body; other symptoms associated with the pain, including nausea, numbness, weakness, etc.; the character of the pain, such as whether is it sharp or throbbing; aggravating factors and activities that worsen the pain; timing of the pain as well as how long it lasts and how constant it is; environments where the pain most commonly occurs, such as in the house or at work; and severity of the pain.
Keeping a pain journal where you track all of these factors in between appointment times may seem tedious, but it can really help you when you need to describe the nature of your pain to a doctor. Your dedication can demonstrate how serious you are about getting the treatment you need.
This can also help you keep an accurate record of your pain for when your doctor asks you about it. This is important because when it comes time for an appointment, some patients feel they are being high-maintenance or dramatic. Russell Portenoy, MD, chairman of the Department of Pain Medicine and Palliative Care at Beth Israel Medical Center in New York City advises doctors to “approach patients who have pain with the assumption that underreporting is a real likelihood.” Many patients underreport because they don’t want to be a bother. With the opioid crisis taking a front seat in the national conscious, many are also wary of being perceived as exhibiting drug-seeking behavior. Of course, these concerns can be stressful, but you should never allow them to get in the way of receiving the quality of care you need and deserve.
While you shouldn’t underreport, you also shouldn’t exaggerate your pain. If you feel like your doctor isn’t taking your pain seriously, there may be a couple reasons for that. First off, doctors only have a limited amount of time with patients, and to treat chronic pain, more time is required. Most physicians also aren’t specifically trained in the most helpful interventions for chronic pain. This sometimes means that they are less likely to fully listen to chronic pain patients because they want to focus on cases where the resolution is more clear-cut. They also may not fully understand the symptoms of your chronic pain and mistakenly attribute them to other conditions. For example, if you complain of pain in your arm, a less experienced doctor may recommend that you wait a few days and see what happens.
In this scenario, Dr. Portenoy suggests making sure that you make it clear to your doctor how pain impacts your life and how your history of it is chronic. Do not shy away from talking about all the ways pain affects you and make sure your answers are specific and detailed. If pain prevents you from being intimate with your partner, keeps you from spending time with friends or family, stops you from working, etc., tell your doctor. While some of this may be uncomfortable to talk about, it can really help drive your point home.
Another good thing to keep in mind is to work on nurturing your relationship with your doctor. It’s hard to make a diagnosis on the first visit and you may have to do some follow ups.
If you still think your doctor isn’t taking your pain seriously or you aren’t seeing the progress you hoped for, see what you can do about getting a referral to a pain specialist. Unfortunately, many doctors aren’t trained in the complexity of pain management. A pain management specialist may be able to get a better feel for the quality of your pain and will have a better idea of the treatments available to you.
At ReclaimAbility Pain Services, our board-certified, fellowship-trained physicians are specialists in pain management. They make it a priority to learn about the specifics of your conditions and work with you to develop a treatment plan that addresses your needs. To learn more about their certifications and backgrounds, visit our team page.